Pain takes many forms: it can be acute (e.g., due to surgical procedures), or chronic (e.g., associated with conditions requiring long-term therapy).1
When talking to your patients, since every patient is different, try to first understand how they are feeling so you can adapt your discourse to their situation:2-4
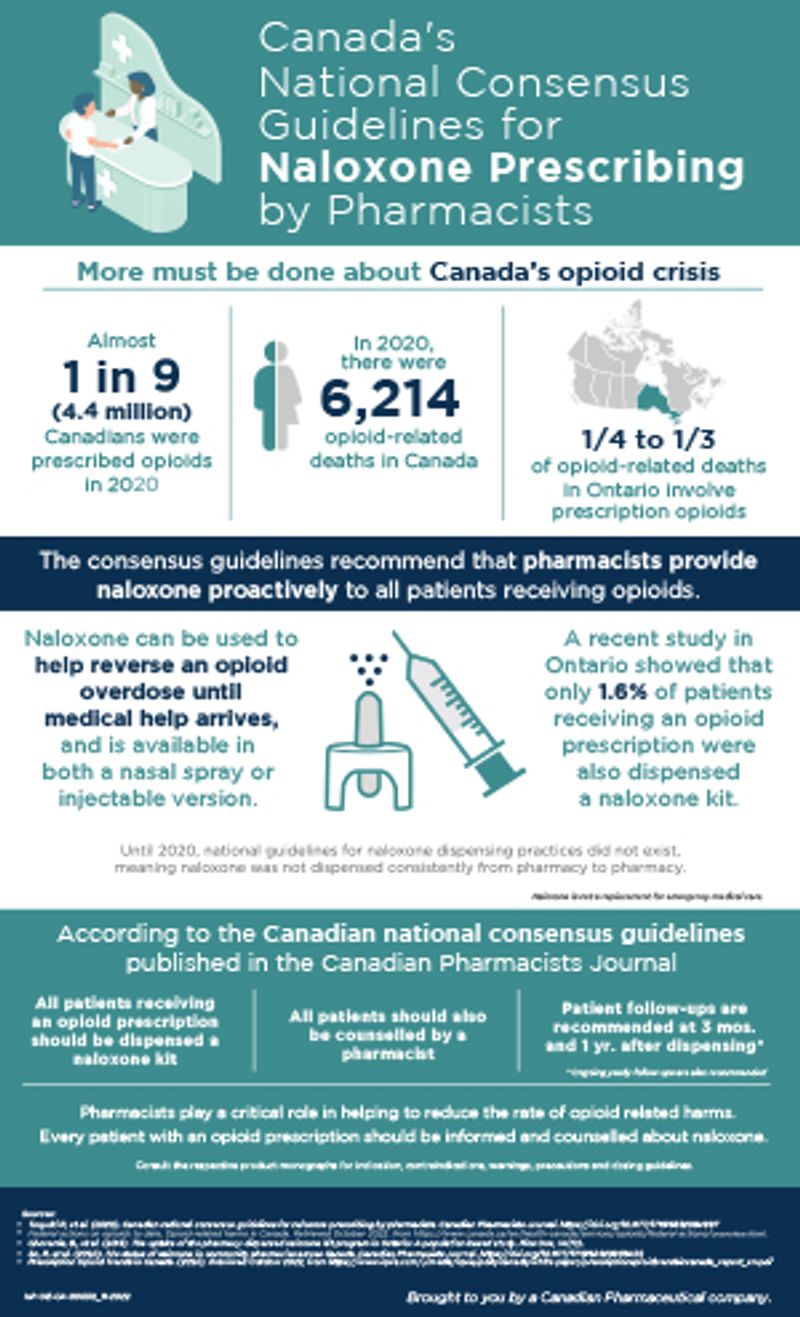
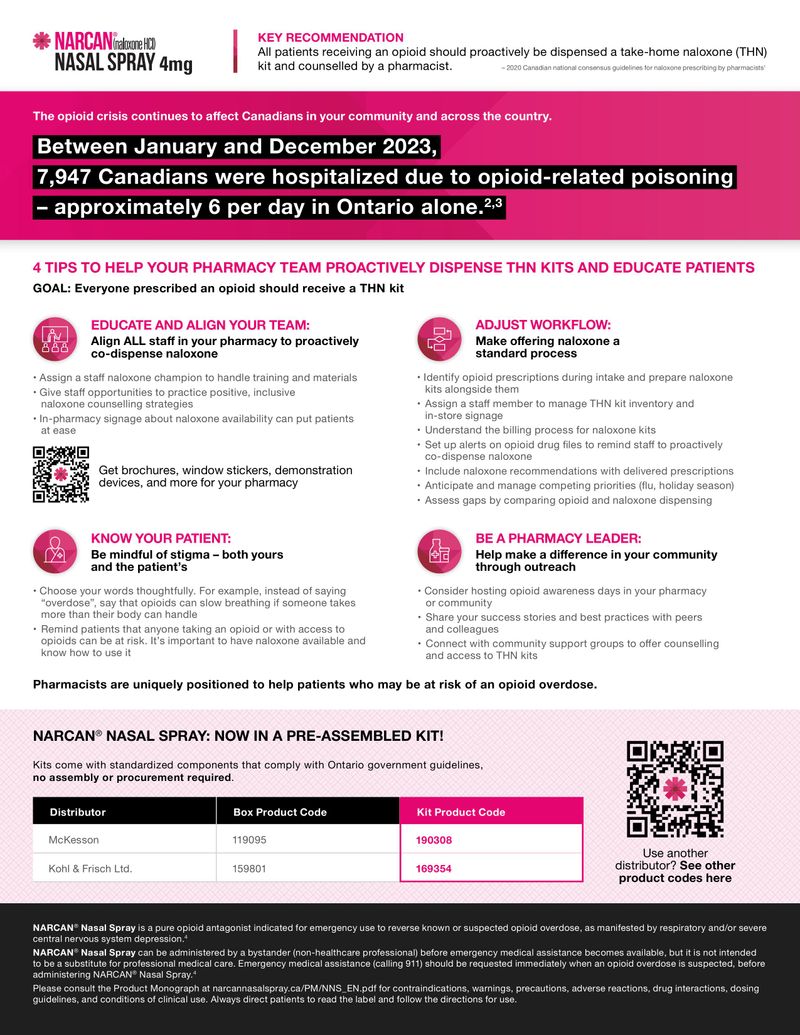
- Some patients may feel uncomfortable or scared of the fact that opioids are being introduced into their treatment plan. Discuss the side effects but try to balance them with the benefits they will experience. Explain the risks of accidental poisoning, as well as the role of naloxone for emergency use to reverse a known or suspected opioid overdose.4-6
- Ask open-ended questions that allow you to assess a patient’s responsiveness in a busy pharmacy environment: e.g., How do you feel about taking this medication?3
- Frame risks in a way that is understandable using analogies: e.g., Think of it like having a fire extinguisher in the kitchen. You hope you don’t need it, but you are prepared if you do.2,6,7
- A study conducted in the United States showed that many patients were not aware their medication was an opioid.8 Ensure your patient understands their prescription; define, in patient-friendly language, what opioids do to the human body and their potential risks.4,5
- Anticipate how to deal with a hostile response: e.g., I’m not an addict. Is that what you see me as after coming to your pharmacy for 5 years? Give me a break! 3
- Put their worries to rest by reassuring them that it is a standard step in your pharmacy to offer a take-home naloxone kit to ALL patients receiving an opioid prescription.5
- Explain that they always have a right to refuse.6
Your patients are counting on you! At the same time, they don’t know what they don’t know! Talk to them about accidental opioid overdose and offer NARCAN® Nasal Spray with every opioid prescription.